A Cross Sectional Study Comparing Blood Parameters for Short Term Adverse Outcome in Syncope Patients
Farizan Tajudin, Nik Azlan Nik Muhamad*
Emergency Department, Medical Centre, National University of Malaysia, Kuala Lumpur, Wilayah Persekutuan, Malaysia
Abstract
Introduction: Mortality from syncope may not be apparent on initial evaluation in emergency department (ED). No reliable tools or clinical decision rule was established risk stratify mortality or morbidity from syncope. This study relates blood parameters with short term serious outcome of syncope. Methods: This was a single centre case control study of adults presenting to emergency department with syncope (n = 98), over 3 months’ duration. Patients particulars, contact profile and blood investigation results were recorded. Patients were called up to ascertain development of serious outcome of syncope within 7 days. Blood parameters such as hemoglobin, hematocrit, serum urea, serum sodium and Troponin I were compared between serious outcome and non-serious outcome group. Result: There was significant difference (p < 0.05) in hemoglobin, hematocrit, serum urea and Troponin I level between the 2 groups of syncope patients. Lower hemoglobin (11.5 ±3.4 g/dL vs. 13.0 ±2.1 g/dL) and lower hematocrit level (34.5 ±9.1 % vs. 38.8 ±5.8 %) were associated with development of short-term serious outcome after syncope. Higher serum urea (9.3 ±8.0 mmol/L vs. 4.3 ±1.2 mmol/L) and abnormally elevated Troponin I (x2 = 15.77; p < .001) were associated with development of short-term serious outcome after syncope. Conclusion: The parameters studied can be a baseline guide for disposition of syncope patient in ED. Further interventional prospective studies are required.
Introduction
Syncope is defined as abrupt transient loss of consciousness (TLOC) with inability to maintain postural tone followed by rapid recovery to preexisting neurologic status1. Emergency Department medical officers (ED MO) find difficulties in determining cause of syncope from initial assessment. The prevalence of syncope presenting to the Emergency Department (ED)range from 0.8% to 2.4% as reported by various studies conducted in the United States and Canada2. Causes of syncope range from very serious condition such as severe aortic stenosis, to benign condition such as vasovagal syncope.
Approximately 10% of patients with syncope develop serious outcome within 7-30 days of their initial presentation.2 Risk stratification is done to recognize patients requiring urgent investigations and hospital admission. Similarly, risk stratification also identifies patient with low-risk condition that can safely be discharged with follow-up hence avoiding unnecessary admission. This can avoid ED overcrowding and prolonged length of stay as reported in Emergency Department of Universiti Kebangsaan Malaysia Medical Centre (UKMMC) previously3,4.
The aim of this study is to relate occurrence of short-term serious outcome of syncope with haematological tests such as haemoglobin level, haematocrit, serum urea, serum sodium and Troponin I5,6. Cardiac biomarkers in particular such as BNP (B-type natriuretic peptide), NT-proBNP (N-terminal proBNP), and hs-cTn (high-sensitivity cardiac troponin) provide useful diagnostic and prognostic information in emergency department patients with syncope. The cardiac markers were significantly higher in cardiac syncope compared to others and provided a 95% sensitivity and specificity7. Results of this tests can assist emergency physicians to risk stratify their patients for disposition, be it an admission for urgent work out or discharge for outpatient follow up. The study provides baseline data for further syncope research in local demography. Outcome of this study will determine which haematological test can correlate to serious outcome in syncope patients, hence can act as a screening or triage tool for emergency care physicians.
Methods
This case control study assesses relation between blood parameters and occurance of serious outcome following syncope. Adult (age>18 years) patients presented to the Emergency Department of Universiti Kebangsaan Malaysia Medical Centre (UKMMC) from April 2019 to May 2020 with syncope or pre-syncope symptoms were recruited. Syncope was defined as transient loss of consciousness and pre-syncope was defined as having a prodromal of syncope. Concurrent seizures, trauma, hypoglycemia, alcohol or substance abuse were excluded from this study.
Researchers conducted briefing to ED staff on the flow and methods of this study. Briefing was repeated regularly throughout the data collection phase. This study did not influence decision making, blood investigations taken and disposition of patients. Blood results that were retrospectively obtained from the online medical system (OMS) were haemoglobin level, haematocrit, urea, sodium and troponin I. Study flow is as depicted in figure 1.
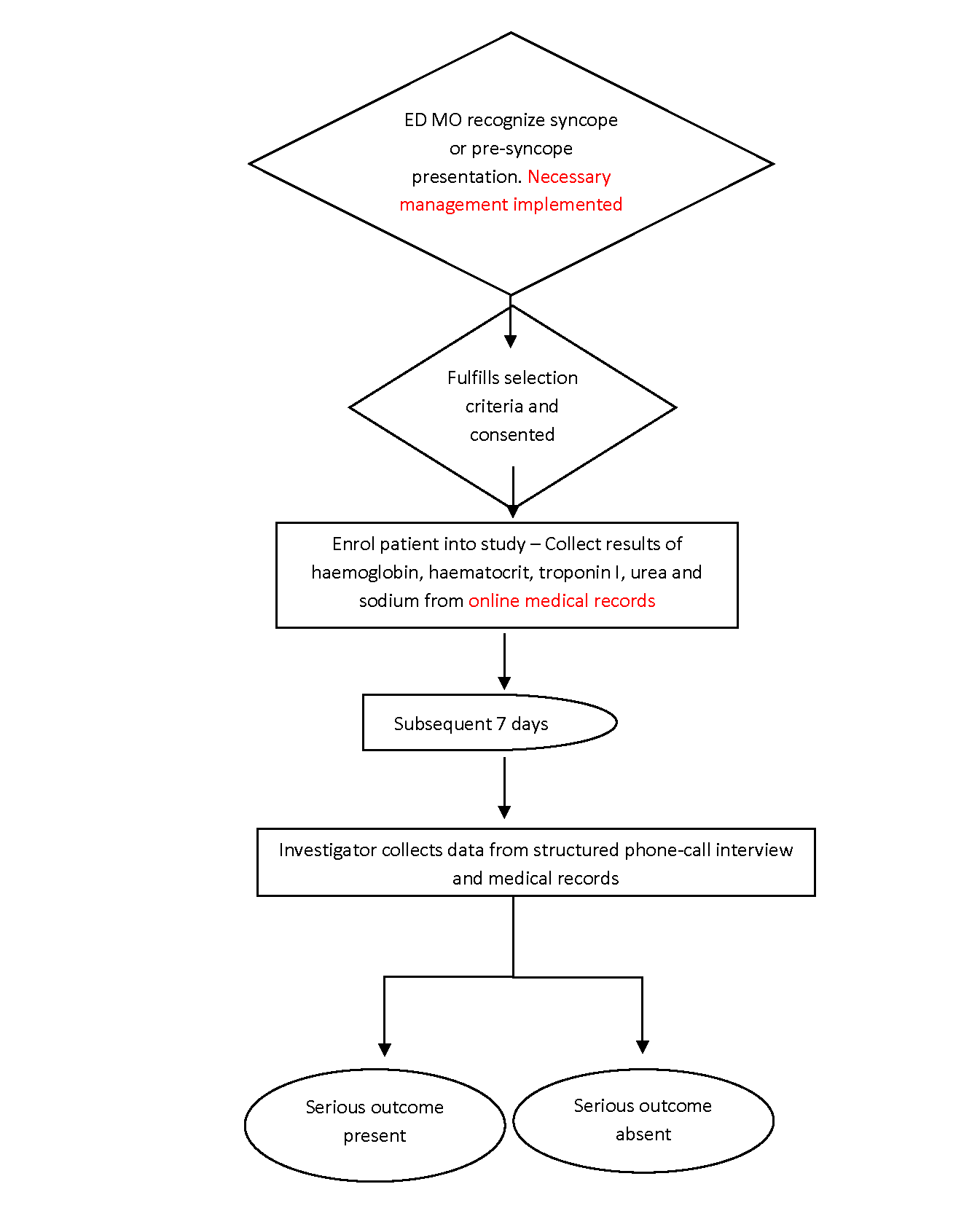
Figure 1: Study flowchart
The date of presentation to emergency department was determined as day 1. Researchers called up patients or relatives following day 7 of presentation. This was done via a structured phone call interview, where contact number was obtained from the medical records. Consent for this interview was obtained during the initial presentation. Questions asked were occurrence of any serious health events including death or sequelae from hospital admission within 7 days of syncope.
Data regarding serious event occurrence within 7 days after the syncope was then collected retrospectively from medical records. Medical records were obtained from either ward or medical records department. Investigator will communicate with treating doctors for patients admitted to other hospitals. Serious outcomes inquired by investigators were:
- Death
- Arrhythmia: ventricular fibrillation, ventricular tachycardia, sick sinus syndrome, sinus pause > 3 seconds, Mobitz type II AV heart block, complete heart block, pacemaker or implantable cardioverter-defibrillator malfunction with cardiac pauses.
- Structural/ Ischemic Heart Disease: aortic stenosis, hypertrophic obstructive cardiomyopathy, left atrial myxoma or thrombus with outflow tract obstruction, myocardial infarction.
- Pulmonary embol
- Aortic dissection.
- Internal hemorrhage or anemia requiring transfusion.
- Recurrent syncope or fall resulting in major traumatic injury (trauma that requires admission or procedural/surgical intervention).
- Permanent pacemaker or defibrillator placement.
- Cardiopulmonary resuscitation.
Correlation was made on the basis of the investigated blood results with serious outcome of syncope.
Sample size calculation
Sample size calculation using Kish et al. estimates population prevalence with good precision8.
n = Z2 x P x (1-P)/d2
Z = Z statistic for a level of confidence
P = expected prevalence or proportion (in proportion of one; if 20%, P = 0.2)
d = precision (d = 0.1)
For confidence level 95%, Z value is 1.96. Estimated prevalence was 50% (P=0.5)
n = (1.96)2 x 0.5 x (1-0.5)/(0.1)2
n=96
From the calculation, our sample should be at least 96 patients. After completed data collection including followed up interview, total sample are 98 patients. Data was tabulated and analysed using Minitab. Two Sample Data Analysis was used to compare mean of blood parameters (hemoglobin, hematocrit, serum urea and serum sodium) between 2 groups of syncope patients (group with serious outcome vs. group with no serious outcome). Mann-Whitney U test was employed due to elevated skewness of blood parameters. Troponin I level was divided into either normal or abnormal value and analysed using chi square test. This is due to the accurate for normal value varied between less than 0.03 to 0.0001 ng/mL.
Results
Ninety-eight patients (n = 98) were recruited into the study. Table 1 shows demography of the sample.
Table 1. Demography of the sample (n = 98)
|
Number / Mean ±SD |
% |
|
|
Age |
50.3 ±20.8 years |
|
|
Gender |
||
|
Male |
54 |
55.1 |
|
Female |
44 |
44.9 |
|
Race |
||
|
Malay |
53 |
54.1 |
|
Chinese |
35 |
35.7 |
|
Indian |
7 |
7.1 |
|
Others |
3 |
3.1 |
Haemoglobin level of the sample population was normally distributed, with mean Hb 12.5 g/dL. The HCT was also normally distributed with mean of 37.2%. Similarly, serum sodium was normally distributed as well with mean of 136.2 mmol/L. However, serum urea distribution was found to be skewed, with median of 4.6 mmol/L, first quartile of 3.4 mmol/L and third quartile of 6.4 mmol/L.
For Troponin I, there are 58 (59.2%) patients with available and required Troponin I result. Mean or median for Troponin I cannot be calculated because negligible levels were reported as <10pg/ml. Hence, Troponin I result was classified by researchers as normal or abnormal based on normal value range. Among the 58 patients who has Troponin I result, 46 (79.3%) of them has normal results, while the other 12 (20.7%) patients have elevated / positive results.
Within 7 days after syncope presentation to ED, 37 patients (37.8%) had developed serious outcome, whereas the rest 61 patients (62.2%) had no serious outcome.
Table 2:. Comparison of blood parameter between 2 groups of syncope (n=98)
|
Variables |
Serious outcome (n=37) |
No serious outcome (n=61) |
Test |
p value |
|
Mean ±SD |
Mean ±SD |
|||
|
Haemoglobin (g/dL) |
11.5 ±3.4 |
13.0 ±2.1 |
Two-sample T |
<0.05 |
|
Haematocrit (%) |
34.5 ±9.1 |
38.8 ±5.8 |
Two-sample T |
<0.05 |
|
Se Sodium (mmol/L) |
135.7 ±5.1 |
136.5 ±4.3 |
Two-sample T |
>0.05 |
|
Se Urea (mmol/L) |
9.3 ±8.06.4 |
4.3 ±1.2 |
Mann-Whitney U |
<0.05 |
|
Troponin I level (percentage sample elevated) |
45.8% (n=24) |
2.9% (n=34) |
Chi square test |
<0.001 |
Table 3. Cross table of variables for chi-square test (n = 58)
|
|
Short term syncope outcome (n=number of patients) |
Total |
||
|
Serious outcome |
No serious outcome |
|||
|
Troponin I level |
Normal level |
13 |
33 |
46 |
|
Elevated level |
11 |
1 |
12 |
|
|
Total patients |
24 |
34 |
58 |
|
Among the 11 patients with elevated troponin, 10 had cardiovascular etiology in which 5 patients had non-ST elevation myocardial infarction (NSTEMI), 2 with ST elevation myocardial infarction, one each of unstable angina, aortic stenosis and dengue carditis. One patient with elevated troponin was reported to have lower gastrointestinal bleed.
Table 4. Type of serious outcome develop after syncope (n = 24)
|
Type of serious outcome |
Frequency |
% |
|
IHD/ structural heart disease |
10 |
41.7 |
|
Arrhythmia |
5 |
20.8 |
|
Severe anemia |
5 |
20.8 |
|
Intracranial pathology |
2 |
8.3 |
|
Others |
2 |
8.3 |
Table 5. End diagnosis of patients with elevated troponin in syncope with serious outcome (n=12)
|
Diagnosis |
Frequency |
% |
|
Acute coronary syndrome: |
|
|
|
STEMI |
1 |
8.3 |
|
NSTEMI |
5 |
41.7 |
|
Type 2 MI (Severe anemia) |
2 |
16.7 |
|
Unstable angina |
1 |
8.3 |
|
|
9 |
75 |
|
Others: |
|
|
|
Severe Aortic stenosis |
1 |
8.3 |
|
Dengue carditis |
1 |
8.3 |
|
Known case of pulmonary hypertension |
1 |
8.3 |
|
|
3 |
25 |
Discussion
From this study it was shown that mean haemoglobin between two groups of outcome following syncope was significantly different (p < 0.05). Lower haemoglobin was found in in the serious outcome group within 7 days after syncope (11.5 ±3.4g/dL vs. 13.0 ±2.1g/dL). In such case, changing from lying to upright position can result in orthostatic hypotension with consequences of reduce cerebral perfusion manifested as syncope. In a single centre, prospective observational study of adults presenting to the emergency department with syncope, haemoglobin level of 9 g/dL and lower was found to be among the independent predictors of serious outcome within 30 days after syncope9.
Hematocrit is the ratio of the volume of red blood cells to the total volume of blood. Likewise, haemoglobin, mean haematocrit in the group who develop serious outcome after syncope was found to be significantly different (p value less than 0.05) than mean hematocrit in the group which did not develop serious outcome after syncope. Lower hematocrit was found in group which develop serious outcome after syncope. Low hematocrit is also associated with low Hb or anaemia. This study finding is consistence with previous study done elsewhere in the development of San Francisco Syncope Rule (SFSR). According to SFSR, hematocrit level of less than 30% is associated with serious outcome within 7 days of syncope5.
For serum urea, this study revealed significant different (p < 0.05) between serum urea in the group who develop serious outcome after syncope, compared to serum urea in the group who did not develop serious outcome after syncope. Higher serum urea was found in group which develop serious outcome after syncope. A systematic review and meta-analysis has found that elevated blood urea nitrogen as one of specific risk factors for serious clinical outcome after syncope10. Thus, serum urea level could aid clinical judgment and should be considered in the development of future prediction tools of syncope. The biological mechanism for relation of elevated serum urea with serious outcome after syncope is not clear. One previous reported that syncope patients in the setting of chronic bifascicular block and associated renal dysfunction have increased mortality than those without renal dysfunction11. Patients with renal dysfunction may bear higher risk for arrhythmias (either because of uraemia or associated electrolyte abnormalities), bleeding, or death (due to comorbidities).
Mean serum sodium in the group who develop serious outcome after syncope, was not significantly different (p > 0.05) than mean serum sodium in the group which did not develop serious outcome after syncope. Serum sodium did not alter risk of developing short term serious outcome after syncope. There is no direct relation has clearly been found between serum sodium with syncope outcome.
For the last variable which is Troponin I, the value lower than 10.0 pg/ml was reported by lab as < 10.0 pg/ml, rather than stating exact value of the Troponin I. Thus, in this study Troponin I level was classified as normal or abnormal value. The value of troponin I above the 99th percentile of Troponin I level for a healthy local population is abnormal. The 99th centile troponin I level for the overall Malaysian population was 23.7 pg/ml, with gender specific values being 29.9 pg/ml and 18.6 pg/ml for male and female, respectively12.
This study used the gender specific value of 99th centile of Troponin I for Malaysian population. Elevated level of Troponin I was significantly associated with short term serious outcome after syncope, mainly due to cardiac causes with p value less than .001. Elevated Troponin I level here was taken as more than 29.9 pg/ml for male and more than 18.6 pg/ml for female. This finding is consistent with other pilot studies which suggest that troponin I may have role in the future risk stratification of syncope, and indeed it may become powerful predictor of serious outcome after syncope6,13.
Limitation
Local prevalence of syncope presentation to ED cannot be established as our study had not recruit consecutive syncope patient throughout the study duration. This is because patient recruitment rate varies throughout the study duration depending on the attentiveness of different ED physicians. Researchers were sometimes not available at the ED to continuously screen for syncope patient.
Time frame for ‘short term’ serious outcome is somewhat arbitrary. Previous researchers have measured outcomes ranging from 7 days to 1 year after the ED index visit. Previous consensus panel work had recommended the use of 30-day outcomes. Ideally, the outcome time frame should maximize the likelihood that a serious outcome is related to the initial syncope episode and affects ED decision making. However, our study took minimal duration for outcome measurement that is 7 days and might missed potential serious outcome after 7 days up to 30 days after syncope.
This study did not exclude patients whom serious outcomes were already identified since at Emergency Department. Including such patients into the study could biases risk prediction toward “obvious” events. For example, upper gastrointestinal bleeding with severe anemia that had been identified at ED as cause of syncope presentation would biases the finding of low Hb with development of serious outcome of syncope.
Another potential bias is incorporation bias, where a test result is used to define the outcome. For instance, an ECG that documents high degree AV block was taken as serious outcome. Despite permanent pacemaker was not being inserted within 7 days after syncope evaluation, patient did not have significant morbidity or mortality, and had no recurrent syncope within 7 days after the index visit.
Mean and median of actual troponin levels were not available due to negligible levels were reported as less than 10 pg/mL. Hence troponin was measures as normal or abnormal. Since this was a case-control study with no intervention, troponin levels were taken when perceived necessary by the medical officer.
Conclusion
Troponin was found to have a significant correlation with serious outcome in syncope, mainly due to cardiac etiology. Hemoglobin and hematocrit at lower than normal levels were also associated with development of short term serious outcome of syncope in our local demography, comparable to previous study for population at other places. Similarly, higher level of serum urea was associated with development of short-term serious outcome of syncope. Further prospective interventional studies, in which all patients with syncope is taken all tests is recommended.
Acknowledgements
We would like to thank Centre of Research in Emergency Medicine (CREM) , Emergency Department, National University of Malaysia Medical Centre for assistance in statistical analysis and dissertation completion.
Authorship
Farizan, T researched literature, conceived the study, involved in protocol development, gaining ethical approval, patient recruitment and data analysis. Nik Azlan NM involved in drafting the article manuscript, critical revision for intellectual concept and revision for publication.
Availability of data and materials
Available with request from correspondence.
Informed consent
Written informed consent was obtained from the patient / relative / caretaker for their anonymized information to participate in this study.
Ethical approval and Human rights statements
Ethical approval for this study was obtained from Research Ethics Committee National University of Malaysia. Ethics approval reference: JEP-2019-202
References
- Brignole M, Moya A, de Lange FJ, et al. Practical Instructions for the 2018 ESC Guidelines for the diagnosis and management of syncope. Heart J. 2018; 39: 43-80. Available from: https://doi.org/10.1093/eurheartj/ehy071
- Benditt DG, Link MS, Mitchell Cohen FI, et al. 2017 ACC/AHA/HRS Syncope Guideline 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients With Syncope. AHA Journal. 2017; 136(5): 60-122.
- Nik Azlan NM, Ismail MS, Azizol M. Management of Emergency Department Overcrowding (EDOC) in a Teaching Hospital. Med & Health. 2013; 8(1): 42-46.
- Ahmad Hanif I, Adila Syafiqah AZ, Chee Ling E, et al. Evaluation of Factors that influnece prolonged Emergency Department stay among admitted patients in University Kebangsaan Malaysian Medial Centre. M-JEM. 2019; 4.
- Quinn JV, Stiell IG, McDermott DA, et al. Derivation of the San Francisco Syncope Rule to predict patients with short-term serious outcomes. Ann Emerg Med. 2004; 43(2): 224–232. Available from: https://doi.org/10.1016/S0196-0644(03)00823-0
- Sun BC, Costantino G, Barbic F, et al. Priorities for emergency department syncope research. Ann Emerg Med. 2014; 64(6): 649–655. Available from: https://doi.org/10.1016/j.annemergmed.2014.04.014
- du Fay de Lavallaz J, Badertscher P, Nestelberger T, et al. B-Type Natriuretic Peptides and Cardiac Troponins for Diagnosis and Risk-Stratification of Syncope. Circulation. 2019; 139: 2403–2418.
- Naing L, Winn T, Rusli BN. Practical Issues in Calculating the Sample Size for Prevalence Studies. AOS. 2006; 1: 9-14. Available from: https://doi.org/10.1146/annurev.psych.60.110707.163629
- Reed MJ, Newby DE, Coull AJ, et al. The ROSE (Risk Stratification of Syncope in the Emergency Department) Study. J Am Coll Cardiol. 2010; 55(8): 713–21.
- Thiruganasambandamoorthy V, Wells GA, Hess EP, et al. Derivation of a risk scale and quantification of risk factors for serious adverse events in adult emergency department syncope patients. CJEM. 2014; 16(2): 120-130. Available from: https://doi.org/10.2310/8000.2013.131093
- Marti-Almor J, Cladellas M, Bazan V, et al. Long-term mortality predictors in patients with chronic bifascicular block. Europace. 2009; 11(9): 1201–1207. Available from: https://doi.org/10.1093/europace/eup181
- Lim SM, Thambiah SC, Zahari Sham SY, et al. Determination of the 99th percentile upper reference limit for high sensitivity cardiac troponin I in Malaysian population 2017. Malaysian J Pathol. 2017; 39(2): 135-140.
- Reed MJ, Mills NL, Weir CJ. Sensitive troponin assay predicts outcome in syncope. Emerg Med J. 2012; 29(12), 1001-3. Available from: https://doi.org/10.1136/EMERMED-2012-201332
