COVID-19 Comorbidity and Non-Communicable Diseases (NCDs) General Reference Hospital (HGR), Niamey, Niger
MAHAMANE SANI Mahamane Aminou1, GBAGUIDI Aichatou Diawara2, MIGITABA Hassane Moctar1, SANI Rabiou1, EMOUD TCHOLI Idrissa3, SALIFOU ALKASSOUM Ibrahim3, FOUMAKOYE GADO Adamou4, BATOURE Oumarou2, OCQUET Sakina5, BRAH Souleymane6, MOUSSA SALIA Amadou6, OUMARA Maman6, TAMBWE Didier2, ANYA Blanche2, Ngozi Idemili-Aronu7, IGWEONU Obianuju7, DANGOU Jean-marie8, ADEHOSSI Eric6, OKEIBUNOR Joseph Chukwudi8, TALISUNA Ambrose8
1Service Endocrinologie, Diabétologie et Nutrition de l’Hôpital Général de référence de Niamey ; BP: 12674, Niamey
2Bureau de la Représentation de l’OMS au Niger, BP: 10739 Niamey, Niger
3Service Surveillance Épidémiologique et Recherche de l’Hôpital Général de référence de Niamey, BP: 12674, Niamey, Niger
4Departement d’Anesthésie réanimation et Urgences de l’Hôpital Général de référence de Niamey, BP: 12674, Niamey, Niger
5Direction des Études et la programmation; Ministère de la santé Publique, Niamey, Niger
6 Service de Médecine Interne Hôpital Général de référence de Niamey, BP: 12674, Niamey
7University of Nigeria, Nsukka, Enugu State, Nigeria
8Bureau Régional de l’OMS pour l’Afrique, PO Box 06, Brazzaville, Congo
Abstract
The COVID-19 infection has highlighted the most vulnerable patients. Indeed, COVID-19 patients suffering from another pathology including NCDs such as Arterial Hypertension (Hypertension), diabetes, cancers and respiratory diseases are paying a heavy price for this pandemic. We undertook a study in Niger to better document this comorbidity in a cross-sectional study that brought together patients hospitalized at the Niamey General Reference Hospital for COVID-19 infection and suffering from one or more NCDs. Among 273 patients hospitalized from March 19 to June 03, 2020, 34.8% had a non-communicable disease associated with COVID-19. The average age of the patients was 55 years (22 years to 94 years) and the sex ratio was 2.64 (72.5 % men and 27.5% women). Hypertension was the most represented NCD with 24.5%, followed by diabetes in 17.9% of cases, respiratory diseases 3.66% and other diseases (Heart disease, Obesity, Dyslipidemia, Gout, Chronic renal failure) with 3%. Health workers were the most affected by the disease with 38.6% of cases. The average consultation time was 3.77 days with extremes ranging from 1 to 8 days. The clinical symptoms characterizing the two main groups of patients (hypertensive and diabetic) were almost identical. It consisted mainly of cough, fever, chills, sore throat and rhinorrhea. According to the WHO clinical criteria for the severity of COVID-19, 34 patients or 16.11% were severe and 177 patients or 83% moderate. The clinical severity of the disease is significantly correlated with the patient's age (over 50 years) and the presence of an NCD associated with COVID-19. A total of 35.8% were hospitalized in intensive care in the NCD and COVID-19 group and 14.6% in the NCD group (p <0.001). The average length of patient hospitalization was 6.87 days overall, it was 7 days in intensive care. In 61.7% of cases the length of hospitalization was greater than 4 days. There was 22.1% in the NCD group and 7.3% in the just COVID-19 group (p <0.001). A total of 90.6% of registered deaths occurred in intensive care.
Introduction
Noncommunicable diseases (NCDs) are emerging diseases that pose a major threat to the world's population, especially in developing countries1. According to the World Health Organization (WHO), NCDs are responsible for more than 70% of deaths and 63% of the global burden of disease2. Persons with existing non-communicable diseases (NCDs) are more vulnerable to health risks due to emergencies and disasters than their counterparts free of any noncommunicable diseases3,4. Those with chronic diseases, such as cardiovascular disease, chronic lung disease, and diabetes have higher vulnerability to disaster induced disruption and stress and significant proportion of mortality in post-disaster phases results from the failure of health care services to cater to the needs of patients with chronic diseases5.
The Corona Virus 19 (COVID-19) pandemic has worsened this already precarious situation. NCDs are a risk factor for the occurrence of COVIS-19 on the one hand and a complication of this disease on the other. Literature show that people with NCDs are at greater risk of severe forms and death from COVID-196. There appears to be a link between the causative agent of COVID-19, hypertension and its cardiovascular complications7. Some studies indicate a high prevalence of hypertension in patients hospitalized for COVID-19, regardless of the geographical focus of the epidemic ranging from 15 to more than 50% in the literature8-10. Other studies have also showed the increased risk of this association.
The impact of COVID-19 on NCD management has recently constituted a major source of concerns, among public health managers globally. The World Health Organization has begun the development of guidelines and recommended actions for people with NCDs during this pandemic11. However, research on the status and disease management of NCD patients in the context of COVID-19 remains very limited in most developing countries3. In Niger there is no data on the extent of NCDs before and during the outbreak of COVID-19. There has also been no research on the coexistence of NCD and COVID-19. The paper therefore examined NCD and COVID-19 comorbidity in order to improve the management of COVID-19 patients in general and those living with one or more NCDs.
Methods
This was a cross-sectional study that made it possible to collect data from patient files and the epidemiological file of COVID-19 patients hospitalized from March 19 to June 3, 2020 in the various care services (Resuscitation and Medicine) of the Niamey General Reference Hospital (GRH). Included were the records of COVID-19 patients treated at the GRH during the period from March 19 to June 03, 2020. The variables studied were epidemiological data: sex, marital status, level of education; clinical characteristics, various associated comorbidities, course, treatment, blood pressure, obesity, glycemia. The diagnosis of COVID -19 infection was made using the PCR test on a nasopharyngeal swab carried out by the Center for Medical Research in Health (CERMES) in Niamey. The severity has been assessed according to the WHO COVID-19 severity criteria8. Patients were classified according to their age, clinical status, paraclinical and presence of NCD and the severity of symptoms (mild, moderate, severe or critical)12.
The data was collected from patient hospital records, the GRH, COVID-19 database. Telephone calls also made it possible to complete certain missing information in the files. The duration of the study was 6 months (June 30 to December 31, 2020).
The data collected was entered and processed using Word, Excel 2016 and SPSS software in version 23 after making an input mask. For the comparison of the results, the statistical tests used were the chi2 considered significant if the probability p <0.05. To carry out this investigation, the agreement of the General Management of the GRH was obtained. Confidentiality was guaranteed and respected during the presentation of results on all survey forms. Informed consent from living patients and families of deceased patients was obtained for further information by telephone and/or interview.
Results
Epidemiological characteristics
During the period of the study from March 19 to June 3, 2020 considered as the first wave of the epidemic in Niger, 273 patients were hospitalized in the various care services of the GRH in Niamey, including 58 patients, i.e. 21, 25% in the intensive care unit and 215 patients or 78.75% in the medical services. The highest number of admissions of COVID-19 cases was observed between April 08 and 12, 2020 with a peak on April 10, 2020. Regarding morbidity, the period from March 31 to April 04, 2020 recorded more of cases with a peak on April 2, 2020 (Figure 1).
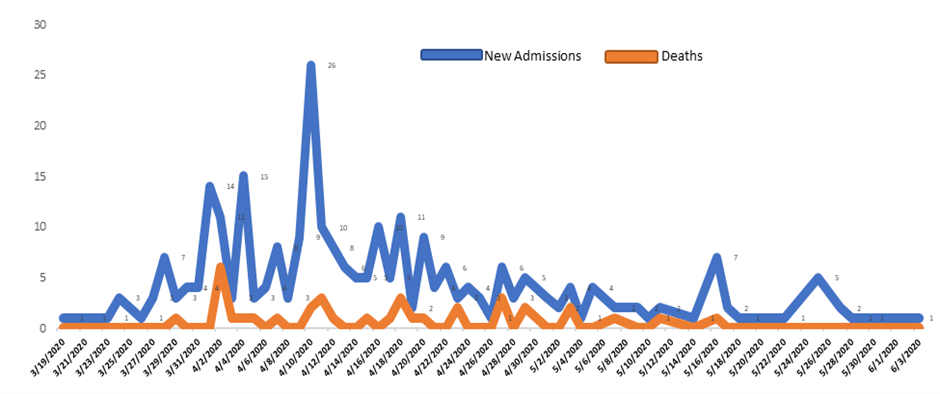
Figure 1: Figure 1: Daily evolution of recorded cases and deaths of COVID-19 at GRH Niamey from March 19 to June 03, 2020
Over thirty-eight percent (38.6%) of the 273 COVID-19 infected persons were health workers. This was followed by other civil servants (13.1%) and retirees (12.5%). Others were traders (11.9%), Housekeepers (6.8%), military officers (5.1%), workers in beauty salons (4.0%), teachers (3.4%), farmers (2.3%), students (1.7%) and drivers (0.6%). Ninety-seven patients (34.79%) presented one or more co-morbidities associated with COVID-19 and 178 patients (65.20%) who did not present any co-morbidity.
Sixty-seven of the COVID-19 patients with NCDs had arterial hypertension. This was followed 49 patients with diabetes, and 10 with respiratory diseases. Another nine had other diseases, including heart disease, obesity, dyslipidemia, gout, leukemia, Chronic renal failure 9 patients. At least 37% of the COVID-19 patients had at least one NCD with comorbidity. See Figure 2.
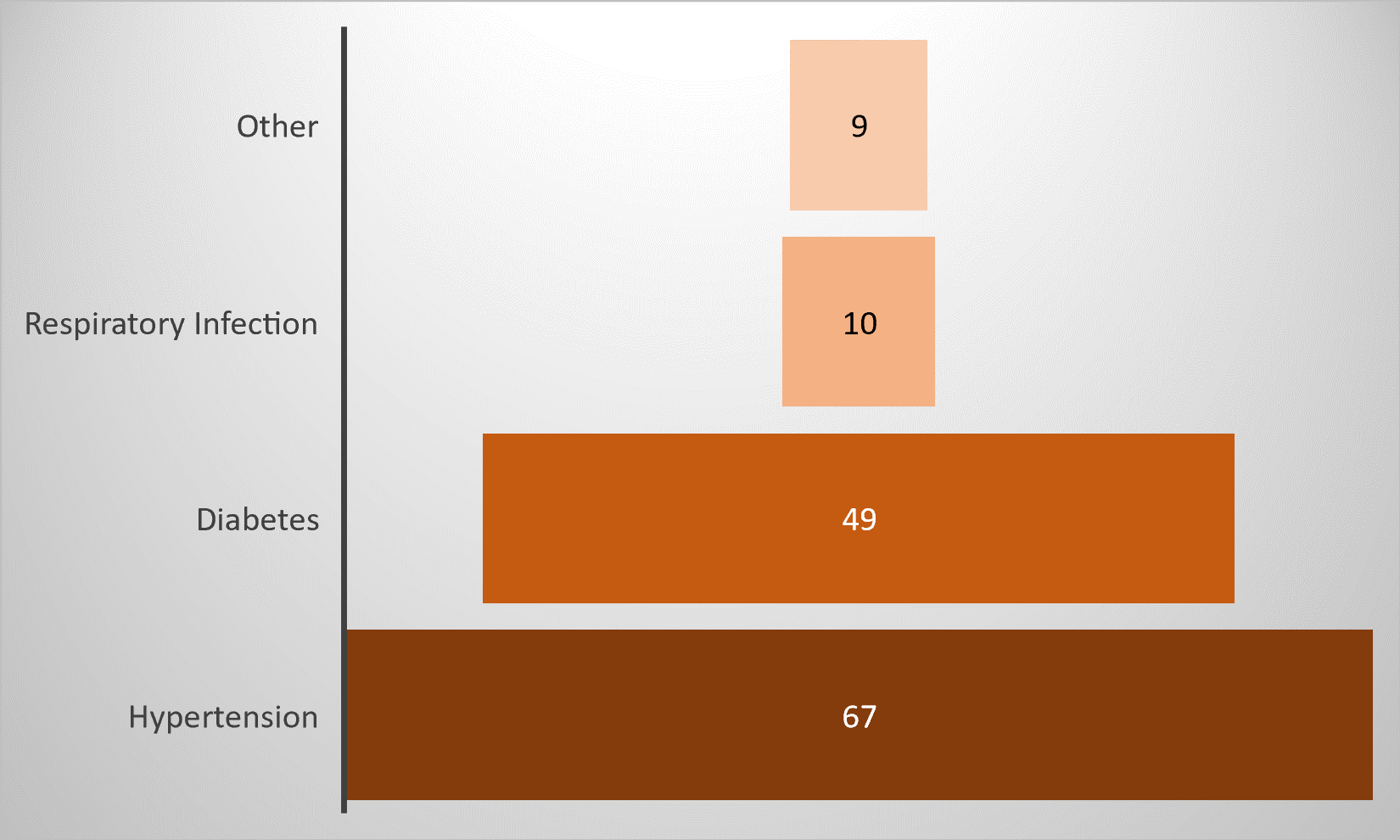
Figure 2: Distribution of co-morbidities associated with COVID 19
The overall distribution of patients by sex shows that men represented 72.52% (198 patients) and women 27.47% (75 patients) of this COVID-19 population with a sex ratio of 2.64. In patients with NCDs men also predominated with 69.5% and women represented 30.5% with a sex ratio of 2.27 in this category.
The overall mean age of COVID-19 patients was 48.91 +/- 17.89 years (12-94 years). Patients with NCD had an average age of 55.78 years while in patients without NCD it was 48.95 years. The extremes were 12 to 90 years for patients without NCD versus 22 and 94 years for patients with NCD. The age group of 50 to 70 years was the most represented in the 2 groups with respectively 35.5% without comorbidities and 50.5% of cases with comorbidities (Figure 3).
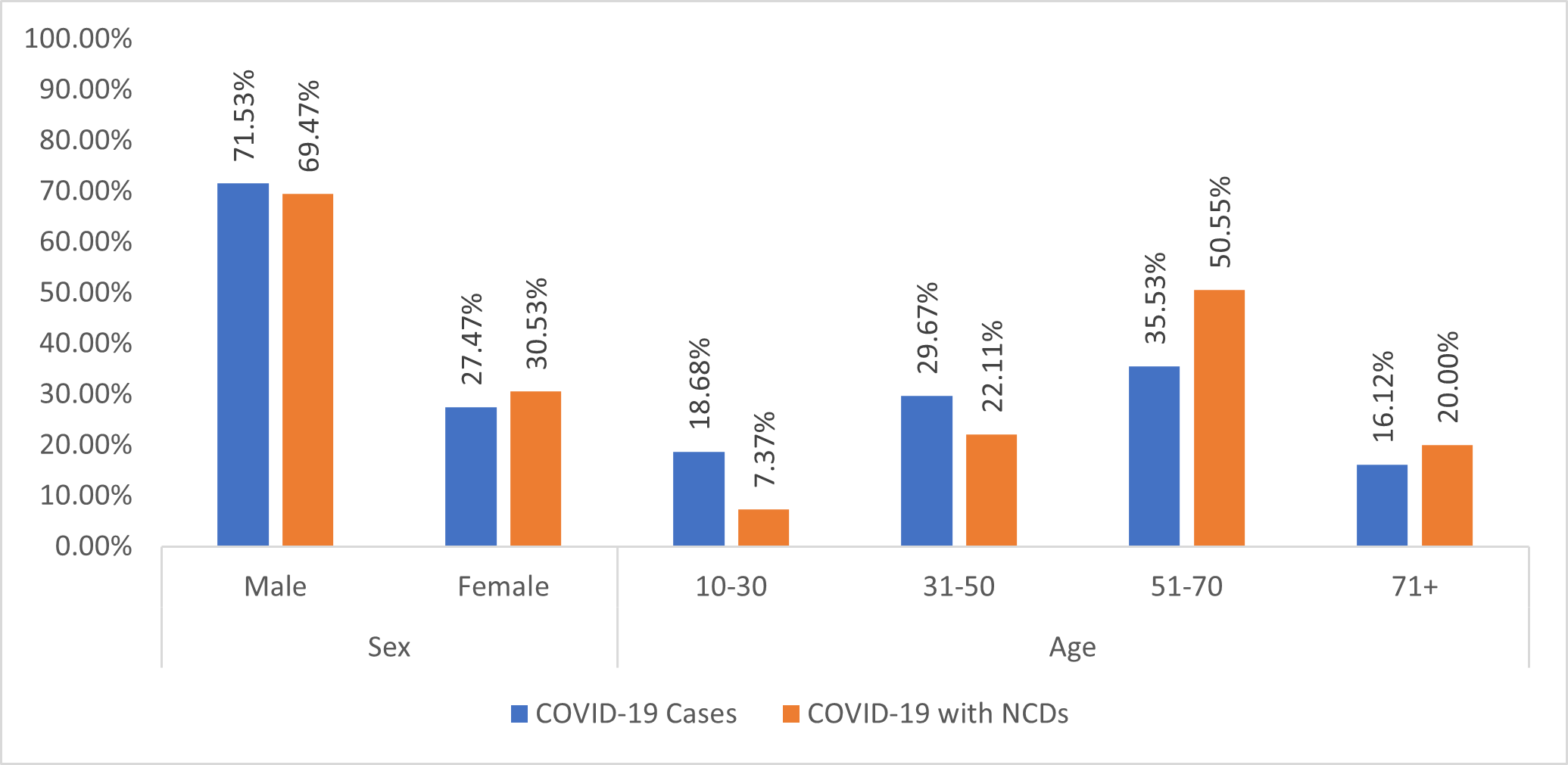
Figure 3: Distribution of COVID-19 cases (N=273) and COVID-19 patients with NCD Comorbidity (n=95) by Sex and Age
Clinical and paraclinical aspects
The average time to see COVID-19 patients was 3.77 days after first symptoms with a range one to eight days. In co-morbid patients, the clinical symptoms characterizing the two main NCDs, hypertension and diabetes, were similar. These were mainly cough, fever, chills, sore throat and rhinorrhea. See Figure 4.
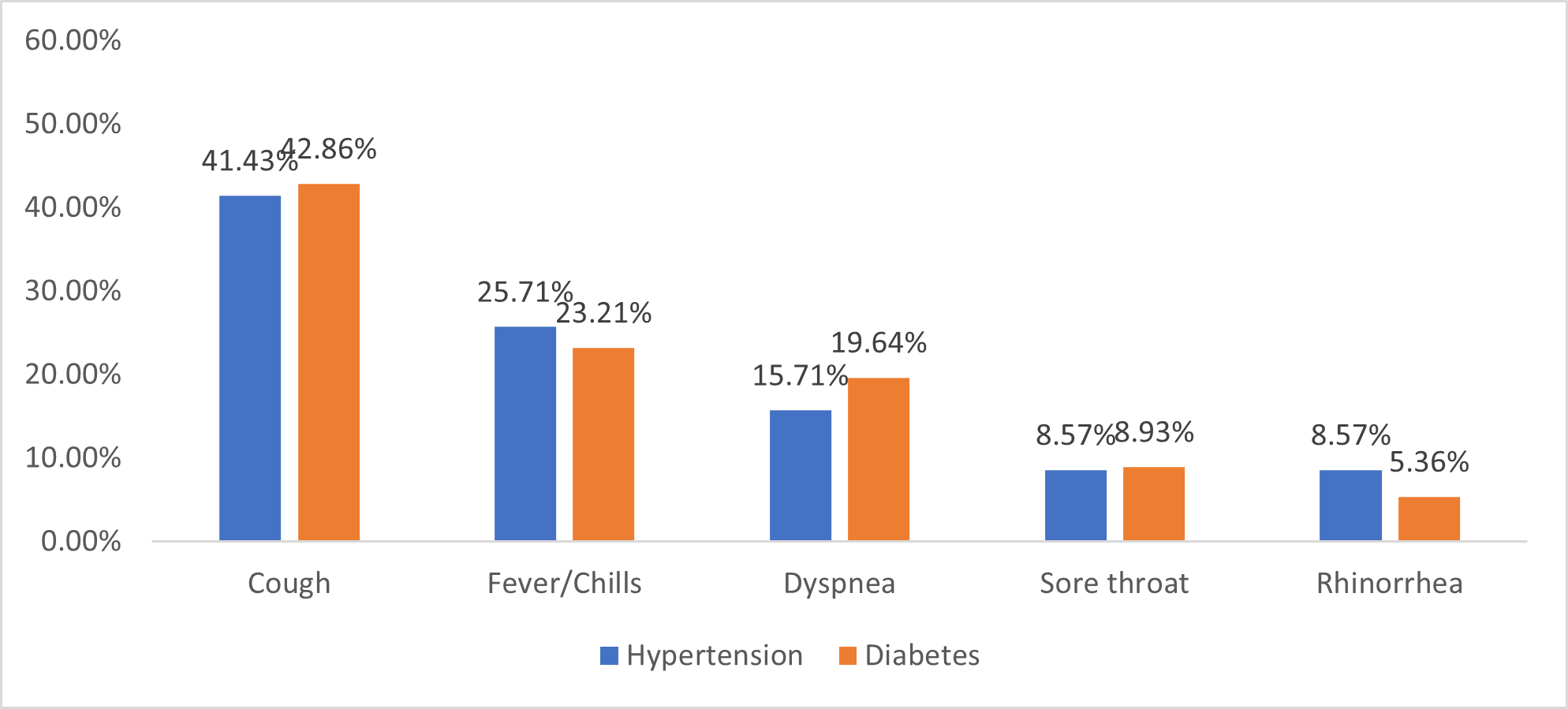
Figure 4: Distribution of COVID-19 patients by symptoms in the group with hypertension and diabetes
Information according to the clinical criteria for classification of the severity of COVID-19 established by WHO was not provided on 62 cases (22.71%). However, on the 211 files (77.29%) which were completed, revealed that in 16.11% (34 patients) the clinical signs were severe and in 83% (177 patients), they were moderate. The analysis showed that there is a significant correlation between the clinical severity of the disease with the age of the patients (over 50 years) and with the association of NCD with COVID-19 (Table 1).
Table 1: Distribution of COVID-19 cases by severity and selected background characteristics
|
Selected background characteristics |
COVID-19 |
OR [IC95%] |
p-value |
|
|
Moderate |
Severe |
|||
|
Age |
||||
|
< 50 years |
99 (55.93%) |
4 (11.76%) |
9.43 [3.40-32.55] |
<0.01 |
|
≥ 50 years |
78 (44.07%) |
30 (88.24%) |
||
|
Sex |
||||
|
Female |
51 (28.81%) |
7 (20,59%). |
1.55 [0.65-04.07] |
0.32 |
|
Male |
126 (71.19%) |
27 (79.41%) |
||
|
Comorbidity |
||||
|
No |
119 (67.23%) |
15 (44.12%) |
2.58 [1.22-5.54] |
0.01 |
|
Yes |
58 (32.77%) |
19 (55.88%) |
||
|
Hypertension |
||||
|
No |
135 (76,27%) |
21 (61,76%) |
1.98 [0.89-4.30] |
0.07 |
|
Yes |
42 (23,73%) |
13 (38,24%) |
||
|
Diabetes |
||||
|
No |
152 (85,88%) |
21 (61,76%) |
3,73 [1,62-8,44] |
0,12 |
|
Yes |
25 (14,12%) |
13 (38,24%) |
||
It emerges from this analysis that adulthood and the presence of comorbidity are statistically associated significantly and have a negative impact on the classification of COVID-19 patients with a p less than 0.05. However, our study does not show a statically significant association between gender and the severity of COVID-19.
Therapeutic and evolutionary aspects
A total of 35.8% were hospitalized in intensive care in the NCD group and 14.6% in the NCD group (p <0.01). The average length of hospital stay was 6.87 days overall. This hospital stay was 7 days in intensive care. In 61.7% of cases, the hospital stay was longer than 4 days. The overall death rate among COVID-19 patients hospitalized at GRH was 12.45% or 34 patients. There were more deaths (22.1%) in the NCD group and 7.3% in the COVID-19 without NCD group (p <0.001). In total 90.6% of patients had died in intensive care. According to NCD, the lethality was 45.8% in hypertensive patients and 54.2% in diabetics.
Discussion
Niger's first COVID-19 patient was registered on March 19 at the GRH in Niamey. Since then, the incidence has steadily increased. The highest number of cases was recorded between 08 and 12 April 2020 with a peak on 10 April 2020. NCDs were therefore the subject of special attention. The prevalence of this combination of COVID-19 and MNT was 34.8% in patients hospitalized at the GRH from March 19 to June 03, considered as the 1st Wave. The results obtained corroborate with the data in the literature. In fact, the studies currently available show a high prevalence of NCDs and COVID-1913,14. In Kenya, around half of COVID-19 deaths have occurred in people with NCDs while in the Democratic Republic of Congo, 85% of COVID-19 deaths have occurred in patients with one or more NCDs15. The prevalence of hypertension was 24% in our series. According to the data in the literature, it varies from 15% to more than 50%15-19. This prevalence was the highest among all the comorbidities in our sample. It seems to be higher in the European series, probably due to an older population. The overrepresentation of hypertension in patients hospitalized for COVID-19 remains very marked in patients hospitalized in intensive care (58%) and among non-survivors (25– 38%)15-19.
South Africa, which records nearly half of the cases and deaths on the continent, found that 61% of COVID-19 patients in hospitals had high blood pressure and 52% had diabetes16. Diabetes was the second most frequently recorded comorbidity in patients with COVID-19 with 17.9% in this population. Data from a study published by the US Center for Disease Control and Prevention (CDC) in the United States shows a prevalence of diabetes of 6% in outpatient COVID-19 patients, 24% in inpatients without intensive care and 32% among hospitalized patients with intensive care20. Based on a meta-analysis of a total of 1382 patient records, it was concluded that people with diabetes were at increased risk for intensive care unit (ICU) admission (OR, 2.79; 95% CI, 1.85–4.22) and mortality (OR, 3.21; 95% CI, 1.82–5.64)21. The higher vulnerability may be explained by the presence of co-morbidities, including cardiovascular disease, and by a reduced immune response to infection22,23.
Age, gender, ethnicity, co-morbidities such as hypertension, diabetes and cardiovascular disease, obesity all probably contribute to the risk of a worse prognosis24,25. People of any age can contract COVID-19, but the elderly (60 years and older) are most affected. In our study, the mean age of patients with NCDs was 55.78 years. Men were more affected than women in our context, which is like the data in the literature25. In a large epidemiological survey in China with 72,314 cases, 51.0% of patients were men26. In a recent report about 1,590 patients hospitalized for COVID-19 in China27, the male gender was 57.3%, and it was 51.3% in the study by Huoshenshan from New York in the United States. USA with 1,780 hospitalized cases. Men represented 72.52% of cases in our study. This finding was indirectly proven by an Italian study of 1591 patients admitted to intensive care units (ICU), of which men represented 82.0%28.
People with NCDs are more likely to have severe symptoms of COVID-19 requiring admission to an ICU28. However, there is no difference in symptoms between hypertensive patients and diabetics. While most COVID-19 patients presented only a mild (40%) or moderate (40%) form of the disease13, it worsens in about 15% of patients, requiring an intake of oxygen, and 5% of patients had a clinically critical condition associated with complications, such as respiratory failure, acute respiratory distress syndrome, septic shock, thromboembolism, and / or multiple organ failure, including acute renal and heart failure29. Old age, smoking30,31 and the presence of underlying NCDs, such as diabetes, hypertension, heart disease, chronic lung disease and cancer, have been described as risk factors for COVID -19 severe and death. In patients with comorbidity, the clinical symptomatology characterizing the two main NCDs (hypertension and diabetes) was similar. These are mainly cough, fever, chills, sore throat and rhinorrhea. However, the initial symptomatology of COVID-19 appears to be more frustrating in the diabetic patient.
In fact, fever is less present in this group of patients, which could induce diagnostic delay16. In our study, 211 of the 273 files contained information relating to the clinical criteria for the severity of COVID-19 established by the WHO13. According to this classification, the distribution revealed that 34 patients or 16.11% were severe and 177 patients or 83% moderate. Known risk factors for rapid deterioration, severe disease and / or increased mortality were: advanced age (> 60 years) and NCDs, such as cardiovascular disease, diabetes, chronic lung disease, cancer and vascular disease cerebral32.
The average length of hospital stay was 6.87 days, almost identical to that of intensive care patients, which is 7 days. There is an excess mortality in the group suffering from NCD (22.1%) compared to the non-NCD group (7.3%) (p <0.01). According to Chinese data covering more than 70,000 cases, the overall mortality from COVID-19 was 2.3% while it was 7.3% in diabetic patients33,34. Diabetic patients therefore appear to be at greater risk of death from COVID-19. Male patients, over the age of 65, appear to be at greater risk not only to COVID-19 but also at a higher risk of developing a critical or fatal clinical condition. Co-morbidities such as hypertension, diabetes, cardiovascular disease and respiratory disease could also negatively impact the prognosis of COVID-19 patients35.
The limitations of this study were related to incomplete records and insufficient certain clinical data, medication and anthropometric measurements such as weight and height in order to assess the patients' BMI.
Conclusion
The COVID-19 pandemic, although recent, has changed the outlook for the management of certain conditions, including NCDs. The combination of COVID-19 and NCD is not only increasing the length of hospital stays, but also the rate of ICU admissions and deaths. In our study, 90.6% of registered deaths occurred in intensive care. To this end, the COVID-19 case management services require capacity building to cope with the management of the second wave started in November 2020 and which seems more intensive. In order to better document this second wave, data collection and analysis is continuing for the prospective part of this study relating to the COVID-19 and NCD comorbidity in Niger.
List of Abbreviations
|
BMI |
Body Mass Index |
|
CERMES |
Center for Medical Research in Health |
|
COVID-19 |
Corona Virus 2019 |
|
GRH |
General Reference Hospital |
|
ICU |
Intensive Care Unit |
|
NCDs |
Noncommunicable diseases |
|
WHO |
World Health Organization |
Ethics approval and consent to participate
Ethical clearance was received from the Nation Ethics Committee in Niamey, and the WHO AFRO Ethics Review Committee. Though the research employed anonymized records of patient in the General Referral Hospital, informed consent was collected from patient and from relatives of the deceased cases.
Consent for publication
Consent to publish was also received from the people during the collection of the informed consent.
Availability and Material
Data supporting the reported results can be got from MAHAMANE SANI Mahamane Aminou, Master Assistant Faculty of Health Sciences, Abdou Moumouni Niamey University, Endocrinology, Diabetology and Nutrition Department at General Hospital of Reference, PO BOX: 12674 Niamey, Niger; Email: aminousani7@yahoo.fr Tel: 0022798556450
Competing Interests: The authors declare no competing interests.
Funding: WHO, Niamey provided financial and technical support for this study
Author Contributions: Conceptualization, M.S.M.A., G.A.D., M.H.M., S.R., and E.T.I.; Methods, S.A.I., F.G.A., Formal Analysis, A.B., M.S.A., O.M., T.D.; Validation, A.B., O.J.C., I.O; A.E., T.A.; Investigation, M.S.M.A., G.A.D., M.H.M., S.R; Resources, A.B.; Data Curation, A.B., M.S.A., O.M., T.D.; Writing – Original Drafting, M.S.M.A., G.A.D., M.H.M., S.R., and E.T.I.; Writing – Review and editing, A.B., O.J.C., I.O.; A.E., T.A.; Supervision, A.B. and O.J.C.; Project Administration, M.S.M.A., G.A.D., M.H.M., S.R., and E.T.I.; Funding Acquisition, A.B.; All authors have read and agreed to the published version of the manuscript.
Acknowledgements
We wish to acknowledge the support we received from the Niamey General Reference Hospital during the data collection and the patients whose data were employed for this paper.
References
- Banque mondiale. L’enjeu de la lutte contre les maladies non transmissibles pour le capital humain, la croissance économique et la santé de la population active https://www.banquemondiale.org/fr/news/immersive-story/2020/02/06/tackling-worlds-deadliest-diseases-can-boost-healthy-workforce-and-economic-growth
- Non-communicable diseases progress monitor 2020. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO.
- Chan EYY, Kim JH, Lo ESK, Huang Z, Hung H, Hung KKC, Wong ELY, Lee EKP, Wong MCS, Wong SYS. What happened to people with noncommunicable diseases during COVID-19: Implications of H-EDRM Policies. International journal of environmental research and public health, 2020; 17:5588; doi:103390/ijerph17155566
- Chan, E.Y.Y. Public Health Humanitarian Responses to Natural Disasters; Routledge: Abingdon, UK, 2017.
- World Health Organization. United Kingdom Health Protection Agency & Partners. Disaster Risk Management for Health: Non-Communicable Diseases. Available online: http://www.who.int/entity/hac/events/drm_fact_sheet_non_communicable_diseases.pdf?ua=1 (accessed on 02 March 2021).
- WHO. Répondre aux maladies non transmissibles pendant et après la pandémie de COVID-19. Rapide tour d’horizon des données probantes sur la COVID 19 et les maladies non transmissibles -WHO 2019-nCoV-Non-communicable_diseases-Evidence-2020.1-fre, 22p
- Cinaud A, et al. Hypertension artérielle et COVID-19. Presse Med Form (2020), 10.1016/j. lpmfor.2020.08.006
- Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Bondi-Zoccai G, et al. Cardiovascular considerations for patients, health care work- ers, and health systems during the Corona- virus Disease 2019 (COVID-19) pandemic. J Am Coll Cardiol [Internet] 2020 [cited 2020 May 1; Available from: https:// linkinghub.elsevier.com/retrieve/pii/ S0735109720346374].
- Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med 2020;8(4): p21.
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York
- Kluge, H.H.P.; Wickramasinghe, K.; Rippin, H.L.; Mendes, R.; Peters, D.H.; Kontsevaya, A.; Breda, J. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 2020, 395, 1678–1680.
- WHO. Prise en charge clinique de la COVID-19 : orientations provisoires. WHO-2019-nCoV-clinical, Mai 2020: 14-16
- Bolin W, Ruobao L, Zhong L, Yan H. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. AGING 2020, 12 (7): 6049-57
- Xiaoyu F, Shen L, Hao Y, Penghao W, Yao Z, Zheng C, Yang L et al. Epidemiological, comorbidity factors with severity and prognosis of COVID-19: a systematic review and meta-analysis. AGING 2020, 12(13) : 12493-503
- OMS Afrique : www.Afro.who.int Les Maladies non Transmissibles augmentent le risque de mourir de la COVID-19 en Afrique. www.Afro.who.int, consulté le 20/01/2021
- Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA 2020 ;323 (16) :1574.
- Loris R, Marco Z, Giovanni Z , Gianluca RRovigo, I 2Ferrara I. Patients with arterial hypertension and COVID-19 are at higher risk of ICU admission COVID-19 Correspondence - e255 , 2p
- WHO. Questions et réponses sur la COVID-19 et l’hypertension artérielle https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and- answers-hub/q-a-detail/q-a-coronaviruses
- Laura O, Michel P. H, Vanessa P, Audrey L, Jean-Paul T, Orsalia A1 et al. COVID-19 et diabeÌte. Louvain Med 2020 mai-juin; 139 (05-06) : 252-257
- Roncon L, Zuin M, Rigatelli G, Zuliani G. Diabetic patients with COVID-19 infection are at higher risk of ICU admission and poor short-term outcome. J Clin Virol. 2020; 127:104354.
- Muniyappa R, Gubbi S. COVID-19 pandemic, coronaviruses, and diabetes mellitus. Am J Physiol Metab. 2020 ;318(5):E736–41.
- Ferlita S, Yegiazaryan A, Noori N, Lal G, Nguyen T, To K, et al. Type 2 diabetes mellitus
- and altered immune system leading to susceptibility to pathogens, especially Mycobacterium tuberculosis. J Clin Med. 2019;8(12):2219.
- Christophe K, Anne Z, Anne W. Diabète et infection aÌ COVID-19 Rev Med Suisse 2020; 16: 939-43
- CDC COVID Response Team, CDC COVID, Response Team, Chow N, Fleming, Dutra K, Gierke R, Hall A et all. Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 'aÌ United States. MMWR Morb Mortal Wkly Rep,2020 3; 69;(13): 382-6
- Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID- 19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020; 41:145–151. https://doi.org/10.3760/cma.j.issn.0254-6450.2020.02.003 PMID:32064853
- Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020; 55:2000547. https://doi.org/10.1183/13993003.00547-2020 PMID:32217650
- Dudley JP, Lee NT. Disparities in age-specific morbidity and mortality from SARS-CoV-2 in China and the Republic of Korea. Clin Infect Dis 2020; published online March 31. https//:doi. org.10.1093/cid/ciaa354.
- Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) – China. China CDC Weekly. 2020;2(8):113-22.
- Alqahtani J.S, Oyelade T, Aldhahir A.M, Alghamdi S.M, Almehmadi M, Alqahtani A.S, et al. Prevalence, Severity and Mortality Associated with COPD and Smoking in Patients with COVID-19: A Rapid Systematic Review and Meta-Analysis. PLoS One. 2020;15(5):e0233147. Epub 2020/05/12.
- OMS. Tabagisme et COVID-19. DeÌclaration de 11 mai 2020. GeneÌve : Organisation mondiale de la SanteÌ ; 2020 (www.who.int/fr/news-room/detail/11-05- 2020-who-statement-tobacco-use-and-covid-19, consulteÌ le 14 mai 2020).
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506. Epub 2020/01/28.
- The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. China CDC Wkly 2020; 2: 113–22.
- Epidemiology Working Group for NCIP Epidemic Response. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin J Epidemiol 2020; 41(2):145-51
- Zheng Z, Peng F, Xu B et al. Risk factors of critical & mortal COVID-19 cases: A systematic literature review and meta-analysis / Journal of Infection 81 (2020) e16–e25
